Articular cartilage
Articular cartilage is a tough layer of smooth white connective tissue that covers the ends of the bones where they articulate with each other within a joint. It is a living tissue which is maintained and repaired by the cells contained within it. It has no blood supply and instead it relies on diffusion of nutrients through the tissue. The reason it appears white rather than pink, is the fact that ir contains no blood vessels. If there was no articular cartilage the bone surfaces would rapidly wear away due the friction that occurs when bone rubs against bone. Articular cartilage is self-lubricating because of its high fluid content which gives it the lowest coefficient of friction of any natural or man-made material.
Types of articular cartilage damage
There are several mechanisms. Direct trauma, repetitive injuries, abnormal direction of loading, fractures, degenerative and inflammatory conditions of the joint and all of these tend to be magnified by exacerbated by the amount of loading of the joint as occurs in obesity.
There is a constant repair process occurring in articular cartilage but it is a slow process and when damage, the repair mechanism can lag behind. When this happens over a prolonged period gradual thinning of the articular cartilage layer occurs.
The repair process
Normally articular cartilage is made of an almost translucent material known as hyaline cartilage which is composed of Type II Collagen and Chondroitin Sulphate. This is only slowly renewed. It develops at its deepest layer and is also maintained by cells throughout the hyaline cartilage known as chondrocytes. If hyaline cartilage is damaged right down to the bone, the blood supply inside the bone is sometime able to start some healing using a specialised scar tissue known as fibro-cartilage. This is a tough material that helps fill in the defect in the hyaline cartilage and which can grow quite quickly. However it is not a good replacement for hyaline cartilage as it is not as resilient to wear and lacks the characteristic low friction properties of hyaline cartilage.
In the later stages of articular cartilage wear bone eventually becomes exposed leading to increased friction and accelerated wear and the development of osteoarthritis.
Outerbridge classification of cartilage damage
Articular cartilage damage is graded according to the Outerbridge classification of cartilage damage described in 1961. This grade is based on the appearance of the articular cartilage when seen at arthroscopy.
-
Grade 0 – normal cartilage
-
Grade 1 – cartilage softening and swelling
-
Grade 2 – partial-thickness loss with fissures on the surface that do not reach subchondral bone or exceed 1.5 cm in diameter
-
Grade 3 – fissuring to the level of subchondral bone in an area with a diameter more than 1.5 cm
-
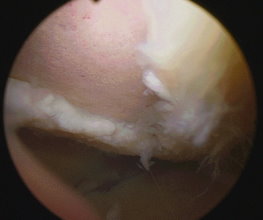
Grade 4 – exposed subchondral bone
|
|
|
A large patch of Grade 4 articular cartilage damage
|
Loose Bodies
Small fragments of cartilage or bone can break off inside the cavity of the knee. These can start off as quite large chunks but more commonly begin as a small loose body that continues growing inside the joint. The characteristic feature is locking or of the joint when the loose body gets jammed between the joint surfaces. This can cause episodes of severe pain, swelling and difficulty in straightening the knee.
A Loose Body in the Knee
Symptoms of articular cartilage damage
These are quite variable but frequently include pain, swelling in the form of fluid within the knee, episodes of giving way, locking or jamming of the joint.
Articular cartilage does have a repair capacity if rested especially in younger people and symptoms can gradually resolve on rest. However more commonly there is gradual worsening of symptoms over time as the damage progresses.
In many cases articular damage goes on to progress to the eventual development of osteoarthritis of the knee.
Treatment
There are a number of potential forms of treatment. Loose bodies can be removed by arthroscopic surgery, and this will help reduce mechanical symptoms and may abolish locking or giving way of the joint. Loose flaky articular cartilage can be removed and surface irregularities can be smoothed down mechanically, a process known as chondroplasty.
Areas of hypertrophic fibrillated cartilage can be smoothed down using radiofrequency ablation. Where bone is exposed a technique known as microfracture can be performed in which multiple small holes are made into the bone surface allowing stem cells from the bone marrow o come through and repair the area with fibrocartilage.
There is a technique that involved taking some good cartilage from a less important part of the knee and moving it to the damaged area in the weigh bearing part of the joint – a technique known as OATS procedure (osteoarticular transfer system). If multiple pieces are moved in this way to form a mosaic of new cartilage pieces in the damaged area it is referred to as a Mosaicplasty. Extensive Mosaicplasties have been largely taken over by newer methods of treatment such as Autologous Chondrocyte Implantation (ACI).
Autologous Chondrocyte Implantation is a technique that harvests cartilage cells from the knee and grows them in the laboratory. The cells multiply and sufficient new cells are grown so that they can be used to cover the area of damage.
TEXT Copyright London Knee Clinic®2014